Dupuytren’s Disease
Dupuytren’s disease, is a progressive medical condition affecting the connective tissue in the palm of the hand. Characterized by the formation of nodules, cords and pits, this disease causes the affected fingers and thumb to gradually bend towards the palm, making it difficult to straighten them. This is known as Dupuytren’s contracture. This can lead to decreased hand function, mobility, and discomfort. Dupuytren’s disease often develops slowly over time and varies in severity among patients, with treatment options tailored to individual needs. Patients often complain of difficulty with tasks such as washing their face, shaking hands and difficulty wearing gloves.
Diagnosis of Dupuytren’s Disease
Diagnosis of Dupuytren’s disease is usually based on a physical examination of the hand and a thorough medical history. The primary goal of treatment for Dupuytren’s disease is to improve hand function and alleviate discomfort, with options ranging from conservative management to surgical intervention, depending on the severity of the condition and the individual patient’s needs. The appearance of the hand is also important and can be improved with treatment.
Prevalence
Dupuytren’s disease is more prevalent in individuals of Northern European descent, particularly those with a family history of the condition. It has been estimated that up to 30% of people of Northern European ancestry may be affected by Dupuytren’s disease to some degree. The condition is less common in people of African, Asian, or Hispanic descent.
In the United Kingdom, it is estimated that around 4% of the adult population is affected by Dupuytren’s disease, with the incidence increasing with age. The condition is more common in men than women, with men being affected about three to five times more frequently than women. This discrepancy is less noticeable over the age of 70 years.
Risk Factors
Several factors have been associated with an increased risk of developing Dupuytren’s disease, including:
Genetics: A strong genetic component has been observed in Dupuytren’s disease, with individuals who have a family history of the condition being at a higher risk of developing it themselves.
Age: The risk of developing Dupuytren’s disease increases with age. It is more common in individuals over the age of 40, with the prevalence increasing further in older age groups.
Gender: Men are more likely to develop Dupuytren’s disease than women and typically experience a more severe form of the condition. The reasons for this gender difference are not well understood but may be related to hormonal or genetic factors.
Lifestyle Factors: Certain lifestyle factors have been linked to a higher risk of developing Dupuytren’s disease, including smoking and excessive alcohol consumption. Both of these factors may have a negative impact on the health of the connective tissue in the hand, contributing to the development of the disease. Additionally, manual labour or trauma may also increase the risk of developing Dupuytren’s disease.
Associated Medical Conditions: Individuals with certain medical conditions, such as diabetes, epilepsy, or liver disease, may be at a higher risk of developing Dupuytren’s disease.
Understanding the risk factors associated with Dupuytren’s disease can help individuals take appropriate measures to reduce their risk of developing the condition or manage it effectively if they are already affected. Early diagnosis and appropriate treatment are essential for maintaining hand function and minimizing the impact of Dupuytren’s disease on an individual’s daily life. Early disease can be effectively treated with less invasive treatments.
Symptoms
The initial symptoms of Dupuytren’s disease are often subtle and may go unnoticed. As the condition progresses, affected individuals may experience the following symptoms:
Nodules: Small, firm lumps (nodules) may develop beneath the skin in the palm of the hand. These nodules are usually not painful but may be tender to touch initially.
Cords: Over time, the nodules can evolve into thickened cords of tissue that extend from the palm towards the fingers. These cords may feel tight or taut and can cause discomfort or aching in the hand.
Finger contractures: As the cords tighten, they gradually pull the affected fingers or thumb towards the palm, making it increasingly difficult to straighten them. This can result in a decreased range of motion, impaired hand function, and discomfort.

Skin puckering: The skin overlying the affected tissue may become puckered or dimpled. Skin pits may become visible in the skin.

Progression
Dupuytren’s disease typically progresses slowly, often over several years. The rate of progression and the severity of the condition can vary significantly between individuals, and it is difficult to predict how rapidly the disease will progress in any given case.
In some individuals, the disease may remain relatively stable, causing only mild symptoms and minimal impact on hand function. In others, the disease may progress more rapidly, leading to significant finger and thumb contracture and impaired hand function affecting everyday tasks.
The condition most commonly affects the ring and little fingers, but it can involve any finger or even multiple fingers simultaneously. The thumbs can also be affected, reducing the span of the hand and the ability to hold or grasp objects. In some cases, both hands may be affected to different extents.
It is advisable for individuals with Dupuytren’s disease to be closely monitored by a specialist with an interest in Dupuytren’s disease to monitor the progression of the condition and make appropriate treatment decisions based on the severity of the symptoms and the impact on hand function. Early intervention and appropriate treatment can help maintain hand function and minimize the impact of Dupuytren’s disease on an individual’s daily life with less invasive treatments and shorter recovery times.
Treatment Options Overview
Observation and monitoring
Observation and monitoring are essential components of the conservative management approach for Dupuytren’s disease, especially in mild cases or during the early stages of the condition. The primary goal of observation and monitoring is to track the progression of the disease, assess its impact on hand function, and determine the most appropriate timing and type of intervention, if necessary.
During the observation and monitoring phase, patients with Dupuytren’s disease can monitor the disease and progression and then undergo an evaluation by a consultant hand and plastic surgeon if they feel the condition is deteriorating. These evaluations may include:
Physical examination: The healthcare professional will carefully examine the affected hand(s) to assess the presence and progression of nodules, cords, and finger contractures. They will also evaluate the range of motion, strength, and overall function of the hand.
Patient-reported symptoms: The patient will be asked about any pain, discomfort, or functional limitations they may be experiencing due to Dupuytren’s disease. This information helps the hand surgeon understand the impact of the condition on the patient’s daily activities and overall quality of life.
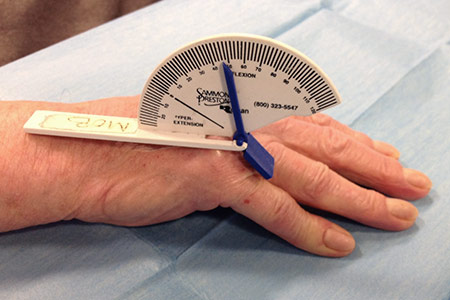
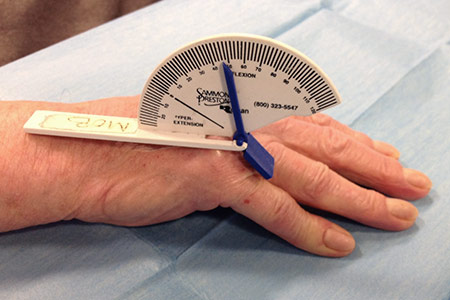
Measurement of contractures: Tools such as a goniometer to measure the angle of the finger contractures is a useful objective measurement to track the progression of the disease over time.
The frequency of these evaluations will depend on the severity of the patient’s Dupuytren’s disease and the rate of progression. For patients with mild symptoms or slow progression, evaluations may be conducted annually or biannually. For patients with more rapidly progressing disease or significant functional impairment, more frequent evaluations may be necessary.
If Dupuytren’s disease is progressing and causing a significant impact on hand function, more active treatment approaches, such as non-surgical interventions or minimally invasive surgical procedures may be recommended. By closely monitoring the progression of Dupuytren’s disease, a specialist can ensure that patients receive the most appropriate and timely care to help maintain hand function and minimize the impact of the condition on their daily lives.
Non-surgical treatments
Non-surgical treatments for Dupuytren’s disease aim to alleviate symptoms, slow the progression of the condition, and improve hand function without the need for invasive surgical procedures. These treatments are often considered in the early stages of the disease or for patients with mild to moderate symptoms. Some of the most common non-surgical treatments for Dupuytren’s disease include:
Occupational therapy: An occupational therapist can work with patients to develop a personalized exercise program to maintain the range of motion, strength, and function in the affected hand. The therapist may also recommend specific stretching exercises or activity modification.
Steroid injections: Corticosteroid injections may be administered directly into the painful nodules. While this treatment can provide temporary relief of symptoms, it is not considered a long-term solution and may not be effective for all patients.
Collagenase injection: This was previously offered as a treatment but the injection is no longer available in the UK.
It is essential to note that the effectiveness of these non-surgical treatments can vary depending on the individual patient and the severity of their Dupuytren’s disease. In some cases, these treatments may provide only temporary relief or may not be effective in preventing the progression of the condition. For patients with more severe symptoms or significant functional impairment, surgical intervention may be necessary to achieve a more lasting improvement in hand function.
Traditional surgical treatments
Traditional surgical treatments for Dupuytren’s disease are typically considered for patients with moderate to severe symptoms or significant functional impairment. The primary goal of surgical intervention is to release the contracted cords, restore finger mobility, and improve hand function. Some of the most common traditional surgical treatments for Dupuytren’s disease include:
Needle fasciotomy: A fasciotomy is a minimally invasive procedure that involves using a hypodermic needle to divide the tight cords through a small “pinhole” incision. The surgeon then carefully cuts through the cords to release tension and allow the fingers to straighten. This procedure is typically performed under specialised skin wheal local anaesthesia and has a relatively short recovery time. This can be an excellent option for those patients with early disease. It has minimal downtime with a quick recovery. The risks include injury to skin, nerve, vessel, tendon, incomplete correction and recurrence. However, the risk of disease recurrence is higher with fasciotomy compared to more extensive procedures.
Before needle treatment for Dupuytren’s disease – unable to lie hand flat on table
Limited fasciectomy: During a limited fasciectomy, the surgeon removes a significant portion of the affected palmar fascia, including the cords and nodules. This procedure can provide long-lasting relief of symptoms and improvement in hand function, but it is more invasive than a fasciotomy and requires a longer recovery period. Subtotal palmar fasciectomy is typically performed under regional anaesthesia.
Extensive fasciectomy: In cases of severe Dupuytren’s disease with extensive involvement of the palmar fascia, an extensive fasciectomy may be necessary. This procedure involves the complete removal of the affected palmar fascia and an invasive surgical treatment for Dupuytren’s disease. It requires a longer recovery period and has a higher risk of complications, but it offers the greatest potential for long-term improvement in hand function. Sometimes joint releases are used as an adjunct to improve the ability of the fingers to straighten.
Dermofasciectomy: Dermofasciectomy is a procedure that combines the removal of both the affected palmar fascia and the overlying skin. This is often performed in cases where the skin has become significantly involved or puckered due to the underlying disease. After the removal of the diseased tissue, a skin graft is typically required to cover the surgical site. This procedure has a lower risk of disease recurrence but carries a higher risk of complications and requires a longer recovery period.
The choice of surgical treatment for Dupuytren’s disease depends on several factors, including the severity of the condition, the patient’s overall health, and the surgeon’s expertise. It is important for patients to discuss the risks and benefits of each surgical option with a specialist hand surgeon to determine the most appropriate treatment approach for their individual needs. Post-operative care, including hand therapy and rehabilitation, is essential for optimizing the outcome of any surgical intervention for Dupuytren’s disease
Focus on minimal access surgery
In recent years, there has been a growing interest in minimal access surgery for Dupuytren’s disease, as these less invasive procedures aim to provide effective treatment with reduced recovery time, lower risk of complications, and minimal scarring. The primary focus of minimal access surgery is to release the contracted cords and improve hand function while minimizing the impact on surrounding tissues and structures.
Until recently an injection of an enzyme called collagenase could be used to treat Dupuytren’s disease. The licence for this product has been removed and it is no longer available as a treatment in the UK.

Needle Aponeurotomy (NA) / Percutaneous Needle Fasciotomy (PNF)
Description of the procedure
Needle Aponeurotomy (NA), also known as Percutaneous Needle Fasciotomy (PNF), is a minimally invasive treatment option for Dupuytren’s disease. This procedure aims to release the contracted cords that cause the fingers to bend towards the palm, thereby improving hand function with minimal impact on surrounding tissues and structures.
The NA/PNF procedure involves the following steps:
Skin wheal anaesthesia: The affected area of the hand is partially numbed using a local anaesthetic to ensure patient comfort during the procedure. It is not possible to completely numb the area as patients need to feed back to the surgeon if they experience and sensations of tingling or nerve pain.
Needle insertion: A fine, sterile needle is inserted through the skin into the thickened cords of the affected palmar fascia.
Cord disruption: Using a careful technique, the needle is manipulated to weaken and divide the cords without the need for a large incision. This process allows the contracted fingers to be gradually straightened.
Finger manipulation: After the cords have been disrupted, the affected fingers are gently manipulated to help improve their range of motion and restore hand function.
Post-procedure care: Following the procedure, patients have a light dressing that can usually be removed 24 hours later.
Benefits and recovery time
The advantages of NA/PNF for Dupuytren’s disease include:
Minimal invasiveness: The procedure involves only small needle punctures in the skin, reducing scarring and the risk of complications associated with more invasive surgical techniques.
Shorter recovery time: Patients typically experience a much faster recovery period following NA/PNF, allowing them to return to their daily activities more quickly.
Reduced cost: NA/PNF is often a more cost-effective treatment option compared to more extensive surgical procedures.
However, there are some potential limitations and risks associated with NA/PNF:
Higher recurrence rate: The risk of disease recurrence is higher with NA/PNF compared to more extensive surgical treatments, as the procedure does not remove the affected tissue entirely.
Suitability: NA/PNF may not be suitable for all patients, particularly those with severe contractures or extensive involvement of the palmar fascia. In such cases, more invasive surgical procedures may be necessary to achieve optimal results.
Potential complications: Although rare, complications such as skin, nerve, vessels or tendon injury can occur. The digit may not go completely straight. The disease may recur.
Patients considering NA/PNF for Dupuytren’s disease should discuss their treatment options with a hand specialist experienced in this technique. By carefully considering each patient’s unique circumstances and needs, the most appropriate treatment approach can be selected to optimize hand function and minimize the impact of the disease on the patient’s daily life.
Why Choose Mary O’Brien for Dupuytren’s Disease Treatment?
Choosing Mary O’Brien for Dupuytren’s disease treatment ensures that you will receive expert care from a highly skilled and experienced consultant hand and plastic surgeon. Her reputation for excellence, patient-centred approach, and commitment to utilizing the latest advancements in treatment make her an ideal choice for individuals seeking effective management of Dupuytren’s disease.
Expertise and experience: Mary O’Brien has years of experience in treating Dupuytren’s disease and possesses the knowledge and skill necessary to address the unique challenges this condition presents. Her expertise in both traditional and minimal access surgical techniques ensures that you receive the most appropriate treatment tailored to your specific needs.
Comprehensive care: Mary O’Brien is dedicated to providing comprehensive care for her patients, addressing not only the physical symptoms of Dupuytren’s disease but also the emotional and psychological aspects. She works closely with a multidisciplinary team of specialists, including hand therapists and support staff, to ensure a holistic approach to your care.
Personalized treatment plans: Mary O’Brien takes the time to thoroughly assess your condition and develop a customized treatment plan that addresses your unique needs and concerns. By considering factors such as the severity of your symptoms, your lifestyle, and your personal preferences, she ensures that you receive the most effective and appropriate treatment possible.
Patient-centred approach: At the core of Mary O’Brien’s practice is her commitment to putting her patients first. She values open communication, ensuring that your questions are answered and your concerns are addressed throughout the treatment process. By fostering a strong patient-provider relationship, Mary O’Brien creates a supportive and nurturing environment that promotes healing and recovery.
Access to cutting-edge treatments: Mary O’Brien stays informed about the latest advancements in Dupuytren’s disease treatment, ensuring that her patients have access to the most innovative and effective therapies available. By staying at the forefront of her field, she can offer you the best possible outcomes for your condition.
High-quality aftercare: Mary O’Brien understands that recovery and rehabilitation are crucial components of successful Dupuytren’s disease treatment. She works closely with hand therapists and other specialists to ensure that you receive the support and guidance necessary for a smooth and effective recovery process.
By choosing Mary O’Brien for your Dupuytren’s disease treatment, you can trust that you are in the hands of a dedicated, compassionate, and skilled professional who will work tirelessly to help you regain hand function and improve your quality of life.
Importance of early intervention and treatment
Early intervention and treatment for Dupuytren’s disease are crucial in managing the condition effectively and preserving hand function. By addressing the symptoms and progression of the disease in its initial stages, patients can achieve better outcomes, require less invasive treatment and reduce the risk of complications. The importance of early intervention and treatment for Dupuytren’s disease lies in the following factors:
Improved hand function: Seeking treatment during the early stages of Dupuytren’s disease can lead to better hand function and overall quality of life. By addressing the condition before it causes significant finger contractures, patients can maintain a greater range of motion and dexterity in their hands, allowing them to continue performing daily activities and hobbies with ease.
Preventing complications: Early treatment of Dupuytren’s disease can help prevent complications, such as permanent joint contractures. Timely intervention reduces the risk of irreversible damage to the hand’s structures, ensuring better long-term outcomes.
Greater treatment options: When Dupuytren’s disease is addressed early on, patients have a wider range of treatment options available. In less advanced cases, minimally invasive procedures like needle aponeurotomy are a good option. As the disease progresses, more invasive surgical options may become necessary, which are typically associated with longer recovery times and higher risk of complications.
Lower recurrence rates: Early intervention and proper management of Dupuytren’s disease can maintain hand function for longer.
In summary, early intervention and treatment for Dupuytren’s disease play a crucial role in effectively managing the condition, preserving hand function, and improving overall quality of life. If you suspect you may have Dupuytren’s disease or are experiencing symptoms, it is advisable to seek a consultation with an experienced hand specialist to discuss your treatment options and develop a personalized plan tailored to your unique needs.
What to expect during the consultation
During a consultation with Mary O’Brien, an experienced consultant hand and plastic surgeon, you can expect a thorough, professional, and compassionate approach to address your concerns related to Dupuytren’s disease. Here is an overview of what to expect during the consultation process:
Medical history and symptom review: Mary O’Brien will begin the consultation by reviewing your medical history, discussing any existing conditions, and enquiring about your symptoms. This information will help her gain a comprehensive understanding of your overall health and the impact of Dupuytren’s disease on your daily life, activities, job and hobbies.
Physical examination: Mary O’Brien will conduct a detailed physical examination of your hands, assessing the presence of nodules, cords, and finger contractures. She will evaluate the range of motion, strength, and function of the affected hand(s) to determine the severity of the condition.
Treatment options discussion: Based on her evaluation, Mary O’Brien will discuss the most suitable treatment options for your specific case. She will provide information about the potential benefits and risks associated with each treatment option, including non-surgical interventions, minimal access surgery, and traditional surgical procedures.
Personalized treatment plan: Together, you and Mary O’Brien will develop a personalized treatment plan tailored to your unique needs and preferences. This plan may involve a combination of therapies, occupational therapy, and medical or surgical interventions.
Preparing for treatment: If you decide to proceed with a specific treatment, Mary O’Brien will provide you with detailed instructions on how to prepare for the procedure, including any necessary pre-operative tests, medications, or lifestyle changes.
Questions and concerns: Throughout the consultation, Mary O’Brien will encourage you to ask questions and share any concerns you may have about Dupuytren’s disease, the proposed treatment plan, or the expected recovery process. Her goal is to ensure that you feel comfortable, well-informed, and confident in your treatment decision.
By seeking a consultation with Mary O’Brien, you can rest assured that you will receive expert guidance, personalized care, and the highest level of professionalism in addressing your Dupuytren’s disease concerns.